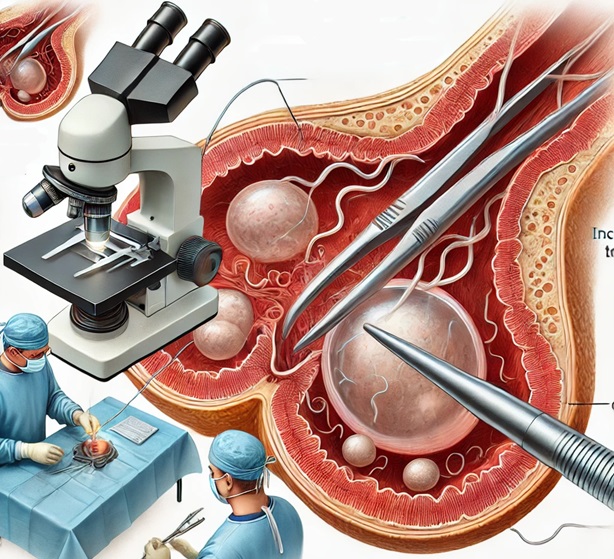
Microdissection testicular sperm extraction (micro-TESE) is a surgical technique used to retrieve sperm from men with nonobstructive azoospermia (NOA), a condition characterized by the absence of sperm in the ejaculate due to impaired or absent sperm production. Recent studies have explored various aspects of micro-TESE to improve outcomes for affected individuals.
Sperm Retrieval Rates and Influencing Factors
A retrospective analysis involving 595 men with NOA investigated the outcomes of micro-TESE and intracytoplasmic sperm injection (ICSI) treatments across different etiologies. The overall sperm retrieval rate (SRR) was 40.3%. Notably, patients with a history of cryptorchidism or mumps orchitis exhibited higher SRRs (84.8% and 84.6%, respectively), while those with idiopathic NOA had a lower SRR (31.8%). These findings suggest that the underlying cause of NOA significantly influences the success of sperm retrieval.
Stepwise Micro-TESE Approach
An innovative stepwise micro-TESE approach was evaluated in a cohort of 64 men with poor prognosis NOA, including those with prior unsuccessful TESE attempts or unfavorable histology. This method involved an initial single conventional TESE biopsy, followed by micro-TESE on the same testis if no sperm were found, and, if necessary, contralateral multiple TESE. The study reported a sperm retrieval rate of 28.1%, indicating that this stepwise approach can be beneficial for patients with challenging cases of NOA.
Second-Look Micro-TESE
The concept of “second-look” micro-TESE has been explored for patients with NOA who had unsuccessful initial micro-TESE attempts. This approach considers the heterogeneity among testicular seminiferous tubules and the possibility of identifying dilated tubules more likely to contain active spermatogenesis. While no reliable positive prognostic factors guarantee sperm recovery, the presence of Y-chromosome AZFa and AZFb microdeletions is considered a negative prognostic factor. Some predictors of SRRs include preoperative follicle-stimulating hormone (FSH) levels and testicular volume, though recent research suggests that increased FSH levels and smaller testicular volume do not necessarily predict adverse outcomes for sperm retrieval.
Clinical Implications
These studies underscore the importance of individualized treatment strategies for men with NOA undergoing micro-TESE. Factors such as the etiology of azoospermia, prior surgical history, and histopathological findings play crucial roles in determining the likelihood of successful sperm retrieval. A tailored approach, considering these variables, may enhance the chances of achieving biological parenthood for affected individuals.
Source : NCBI.NLM.NIH.GOV BMCUROL.BIOMEDCENTRAL.COM PMC.NCBI.NLM.NIH.GOV